Achilles tendon
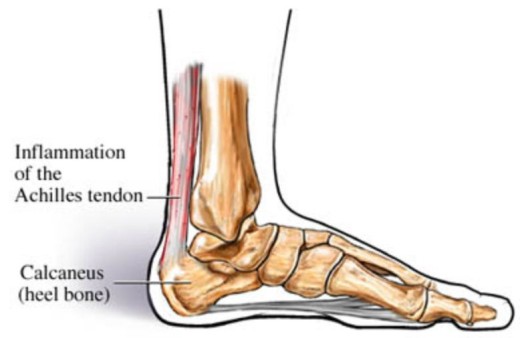
Achilles tendinopathy can be an acute or chronic condition. Acute conditions occur over a period of a few days and are usually a result of increase in activity, whereas chronic condition occurs over a longer period of time. Usually, degeneration of the tendon leads to decreased strength leading to injury. The condition can occur at the point of attachment to the heel or midway up the tendon and healing of the tendon is slow due to the poor blood supply.
The cause of Achilles tendinopathy is usually repeated tiny micro traumas to the tendon, followed by incomplete healing, occurring over time building up to injury. For example, overuse with excessive training, training in inappropriate footwear, spending a lot of your training running uphill, or constantly wearing high heels that shortens the Achilles tendon, then training in flat shoes causing excess strain on the tendon.
Achilles tendinopathy is more common in men than women, and more commonly occurs to those over 40. Symptoms begin gradually with pain at the back of the ankle especially when exercising, running uphill or climbing stairs. Pain will be worse in the morning or after a prolonged rest. The tendon will be tender on palpation and there may be some swelling and thickening of the tendon.
Diagnosis will be made by a doctor and you may have an ultrasound or MRI to rule out an Achilles tendon rupture. Self treatment will begin with R.I.C.E. Resting the foot will prevent further injury whilst applying ice and elevating the foot will help with swelling and pain. Ice should be wrapped in a towel before applying, do not apply ice directly to the skin. A compression bandage may help be giving support to the foot and ankle. Your G.P. may also prescribe painkillers to help alleviate symptoms. Always consult your doctor before taking medication to ensure they are suitable.
An extensive rehabilitation program will be recommended by your physiotherapist. The physio may use different techniques including massage, acupuncture, and ultrasound or taping. They will also recommend a series of stretching and strengthening exercises and advise of when to begin your training regime. It may take as long as 3 months to return to high impact sport. The physiotherapist will also observe your gait to assess if you have a mobility issue i.e. flat feet, which you may need an orthotic shoe insert to prevent increased pressure on your Achilles tendon.
Symptoms are usually gone in 3-6 months using these methods. If after this time you are still experiencing problems, there are other methods available but generally at the moment not on the NHS. These include extracorporeal shock-wave therapy, using sound waves to promote healing, Injection using autologous (your own) blood, which stimulates healing and using a glyceryl trinitrate patch for symptom relief and healing. These treatments are only recommended after a thorough consultation.
Approximately 1 in 4 people with Achilles tendinopathy will get no relief from any of the above and will need surgery. This usually removes nodules or adhesions on the tendon and a rehab program by a physiotherapist will follow post-op.
For more fun volleyball news click here.
Check out the news from our Interviews section, every Tuesday a new story! Tomorrow read about
Aleh Akhrem: we was need this victory